Mobetron: The Surgical Enhancement for Patients with Pancreatic Cancer
Surgery isn’t an option for every patient diagnosed with pancreatic cancer. But with improved systemic treatment and adding electron IORT with the Mobetron®, more patients than ever before are eligible. And we know that those who are treated surgically have a higher chance of survival.
As an oncologist, you also know that despite the improvements made in the fields of surgery, chemotherapy and radiation therapy, pancreatic cancer remains one of the most lethal malignancies facing patients and physicians today. In fact, pancreatic cancer is the fourth most common cause of death from cancer among men and women. Historically, median survival rates of five years or more are nothing short of dismal. Rates of recurrence and relapse demonstrate a sobering reality.
Surgery is the best chance for a cure and yet for so many patients, there is no surgical option. Why? Well, given the nature of the disease, it is estimated that 40% of patients present with locally-advanced unresectable or borderline resectable case. According to the recent publication “Intraoperative Radiotherapy in the Era of Intensive Neoadjuvant Chemotherapy and Chemoradiotherapy for Pancreatic Adenocarcinoma”, at presentation, only 10-20% of patients with pancreatic adenocarcinoma have potentially resectable cancers. Even with resection, only 20-30% of patients will survive five or more years.
In most cases, it’s a matter of time.
The Mobetron presents a compelling new strategy in the fight against pancreatic cancer. Used by the leading cancer physicians and radiation oncologists in the world’s most innovative and trusted hospitals, clinics and academic centers, the Mobetron is the first portable, self-shielded electron linear accelerator designed to deliver Intraoperative Radiation Therapy (IORT) to cancer patients during surgery.
For surgical oncologists, Mobetron can be a critical collaborative enhancement in efficiently and effectively delivering an ablative dose of radiation directly to the tumor bed at the optimal biologic time. This ensures confidence among surgical specialists that targeted microscopic and residual cancers may have been managed during the intervention and that the procedure has effectively expanded the margins of locally-treated tissue. Mobetron can make a significant difference in the clinical outcome for this disease.
With Mobetron, the physics of electron IORT results in greater precision, greater control and greater promise. While Mobetron has a proven history of treatment of breast and other cancer indications, in pancreatic cancer, the numbers are more than encouraging. For surgeons and radiation oncologists alike, Mobetron can provide a unique advantage.
Pancreatic Cancer Treatment Demonstration
Because advanced progression in local tumors causes greater morbidity and mortality among pancreatic cancer patients, significant attention has been paid to the role of localized radiation therapy. The approach has resulted in improved outcomes, but even then, rates of failure can be as high as 50 to 80%. And the location of the pancreas and its proximity to bone marrow, spinal cord, kidneys, liver and intestines means that precision is critical. IORT with electrons makes surgery possible for more patients. Having treated thousands of patients with pancreatic cancer, Mobetron is the standard in IORT.
Pancreatic Cancer: The Hard Facts
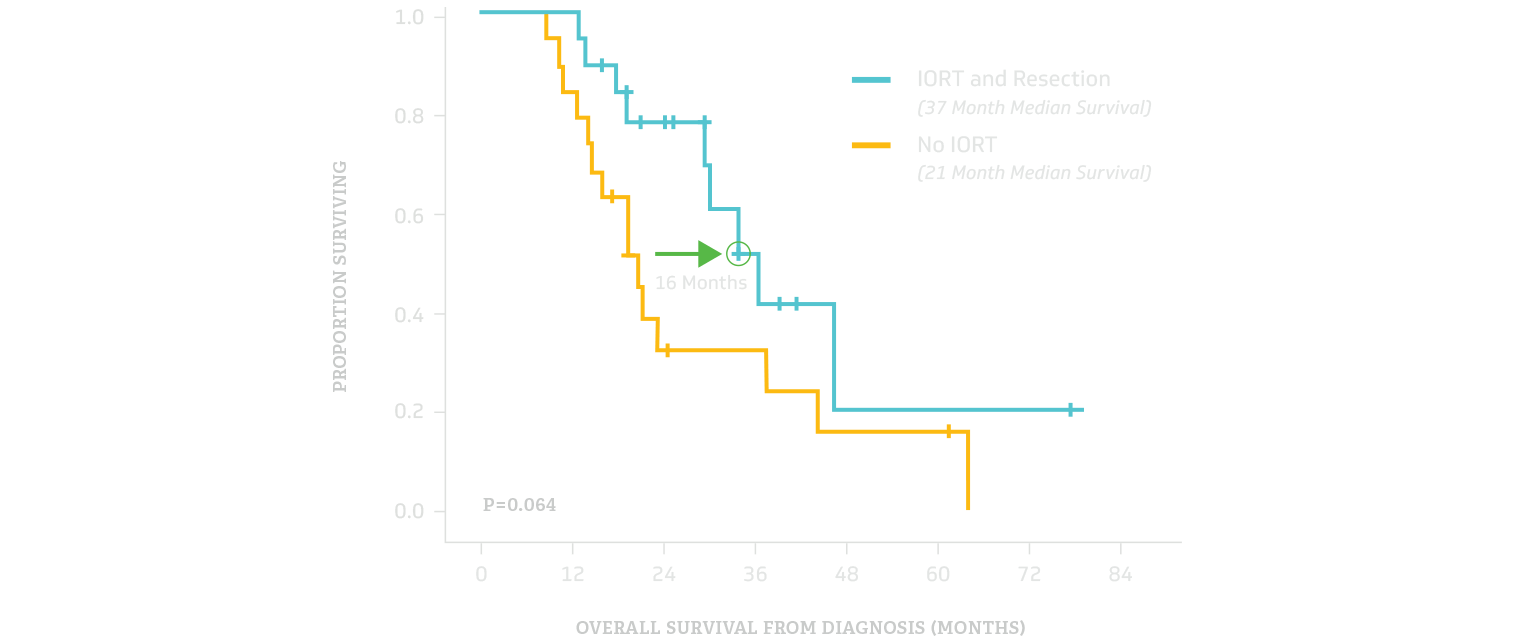
IORT Appears to Mitigate the Effect of R1 Resection Among Patients With Pancreatic Ductal Adenocarcinoma (PDAC)
A recent study published in the Annals of Surgical Oncology reveals neoadjuvant therapy with Intraoperative Radiation Therapy (IORT) may improve survival rates among Pancreatic Ductal Adenocarcinoma (PDAC) patients by reducing the effect of microscopically positive tumor margins.
Pancreatic cancer surgeries are often very challenging procedures and several published studies have demonstrated a correlation between R1 resections and lower overall survival in pancreatic cancer patients.
In a retrospective study of 201 patients, Sekigami Y., et al. from Harvard’s Mass General Hospital reported that:
- There was no statistically significant difference in overall survival between R0 and R1 resections when implementing an ablative dose of IORT to treat suspect margins.
- The median overall survival was 76% longer (37 months vs 21 months) for patients with an R1 resection that received IORT compared with surgery alone.
- There was no significant difference between the 30-day major complication rates for those who received IORT and those who did not.
This encouraging data continues to strengthen the data supporting the role of electron beam IORT in the multidisciplinary treatment of pancreatic cancer.
Overall Survival Comparison
SOURCES:
- Annals of Surgical Oncology, “Intraoperative Radiation Mitigates the Effect of Microscopically Positive Tumor Margins on Survival Among Pancreatic Adenocarcinoma Patients Treated with Neoadjuvant FOLFIRINOX and Chemoradiation” by Yurie Sekigami, et al.
Electron IORT has been used to successfully treat multiple cancer indications for nearly 50 years and has treated thousands of pancreatic patients. IORT is not experimental. It is proven.
The Role of IORT in Pancreatic Cancer Treatment
IORT delivers radiation precisely to the tumor bed after surgical resection. The exacting nature of this approach alleviates various concerns for both the physician and patient alike.
Designed to deliver high doses of electron radiation therapy, IORT excludes part or all of the nearby dose-limiting sensitive structures. With it, the effective radiation dose may be increased and local tumor control potentially improved. Because local failure rates are as high as 50–80% in patients with resected and locally advanced cancerous tissue, this is an imperative.
Recent results of studies at University of Kyoto in patients with resection followed by IORT suggests that IORT is an ideal therapeutic strategy for pancreatic cancer. This is attributable to advantages in delivering high doses of radiation to areas at risk for microscopic disease, while sparing critical organs and reducing the possibility of inducing toxicity. (Source: Radiation Oncology)
Survival Grouped By Resection Status And IORT
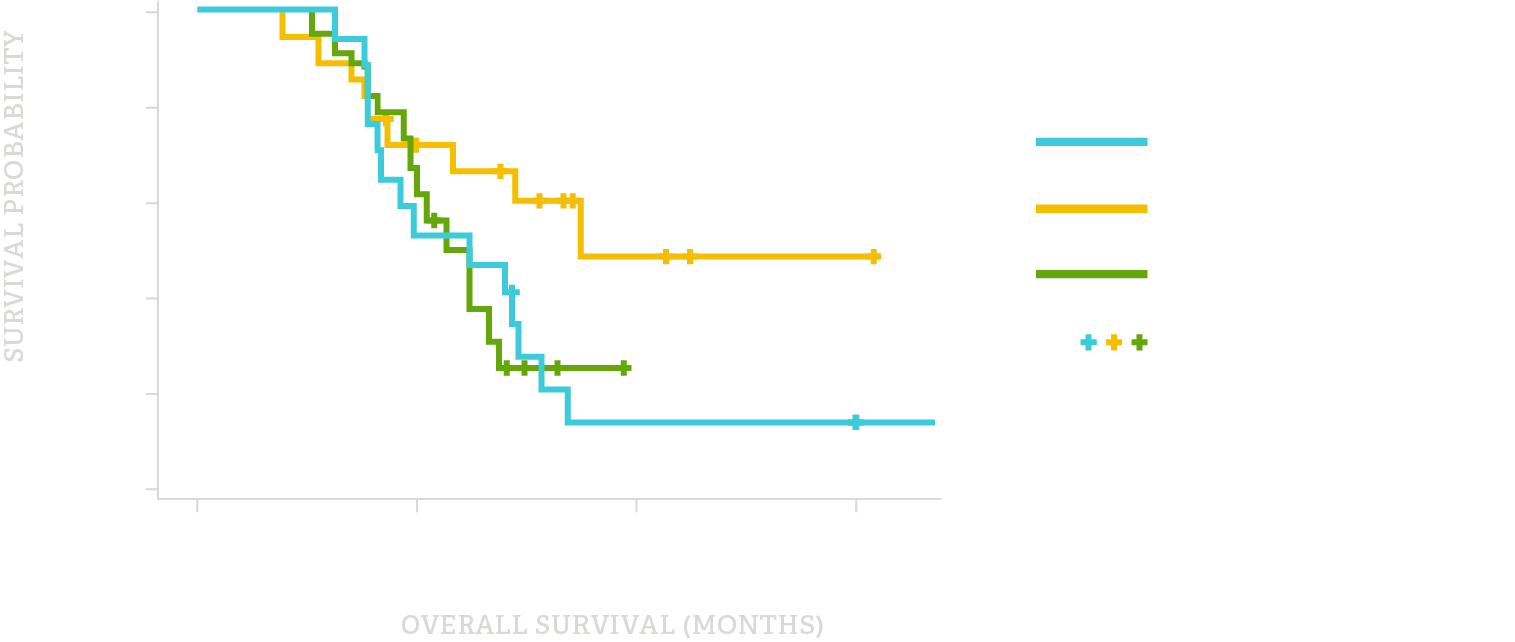
Combining Electron IORT with Improved Systemic Therapy
While the clinical research is still in an early phase, electron-beam IORT may increase the overall survival rates of patients with locally advanced, unresectable pancreatic cancer, according to researchers from Harvard and Massachusetts General Hospital (MGH) published in the American Journal of Clinical Oncology.
In the first study of its kind, MGH researchers incorporated the drug combination FOLFIRINOX into an intensive neoadjuvant treatment protocol, which included electron beam IORT during surgery. The use of IORT was “associated with encouraging median survival rates” with patients who underwent surgery and IORT experiencing a 43% increase in their median overall survival rate (35.1 months) compared to patients who did not receive IORT after surgery (24.5 months).
Improved outcomes with FOLFIRINOX or gemcitabine with nab-paclitaxel in the treatment of metastatic pancreatic adenocarcinoma (PDAC) have prompted incorporation of these regimens into neoadjuvant treatment of locally advanced unresectable PDAC.
According to the authors, another ‘particularly intriguing’ finding was that patients whose cancer could not be surgically removed appeared to benefit from receiving IORT alone with a reported median survival of 24.8 months.
According to the authors, another “particularly intriguing” finding was that patients whose cancer could not be surgically removed appeared to benefit from receiving IORT alone with a reported median survival of 24.8 months.
For decades, electron IORT has been used for locally advanced and recurrent cancers, achieving excellent clinical results in both local control and survival, especially in colorectal cancers, head and neck cancers, GYN cancers, and sarcomas. These latest results indicate electron IORT may do the same for pancreatic cancer patients.
It should be noted that radiographic assessment after intensive neoadjuvant treatment is challenging and may not be representative of resectability. As systemic therapy improves, the ability to achieve local control will likely play an increasing role in improving patient outcomes. The role of radiotherapy will need to continue to be reevaluated.
Further, the efficacy of external beam radiation therapy (EBRT) in pancreatic cancer is limited by the inability to deliver adequate doses of irradiation secondary to the dose tolerance limits of small bowel, spinal cord, stomach, kidney, and liver.
While these numbers are modest, they are an improvement and encouraging clinical studies to be launched. Clinical research will draw more attention to IORT’s role in treating pancreatic cancer and more patients undergoing surgery in more participating hospitals to treat the disease. Perhaps as many as 7,000 to 8,000 patients (of the 55,400 new cases) will receive restive surgery. By bringing more eligible patients to surgery, treatment with Mobetron has the potential to save more lives. It is premature to consider this a cure, but it is certainly a clear path to the cure that will come one day.
SOURCES:
- Radiation Oncology, “Intraoperative radiation therapy (IORT) in pancreatic cancer” by Robert Krempien and Falk Roeder (Link)
- “Intraoperative Radiotherapy in the Era of Intensive Neoadjuvant Chemotherapy and Chemoradiotherapy for Pancreatic Adenocarcinoma” by Florence K. Keane, MD, Jennifer Y. Wo, MD, Cristina R. Ferrone, MD, Jeffrey W. Clark, MD, Lawrence S. Blaszkowsky, MD, Jill N. Allen, MD, Eunice L. Kwak, MD, PhD, David P. Ryan, MD, Keith D. Lillemoe, MD, Carlos Fernandez-del Castillo, MD, and Theodore S. Hong, MD (Link)
- American Cancer Society
- U.S. National Library of Medicine
Mobetron is an effective, productive, and safe solution. We have the numbers to prove it.
Bottom-line Productivity In The OR with Mobetron
Mobetron treatment is optimized for the OR, thereby maximizing physician productivity. For Oncologists, Mobetron enables more of their patients to benefit from comprehensive multidisciplinary treatment including surgery, radiation therapy and chemotherapy.
For facilities, the portable, self-shielded design of Mobetron requires absolutely no costly bunker construction or retrofitting. Its soft-docking laser-alignment system gets surgical teams working quickly. And two-minute integrated treatment times equate to more procedures during the course of each daily unit.
Further, with Mobetron, there is no increase to the average hospital inpatient stay.
These are bold claims. But oncologists who use Mobetron will tell you that the dose and volume precision and uniformity in dosimetry are keys to their success in the operating room. Combine that with shorter treatment cycles and minimized impact to healthy tissue, and Mobetron is an effective, productive, and safe solution. We have the numbers to prove it.
The Next Step In Pancreatic Cancer
At IntraOp, we know that innovation represents the future in the battle against pancreatic cancer. Now we know more is possible with Mobetron. The world’s best oncologists tell us it’s a necessary component in their toolkit. Healthcare executives tell us Mobetron is a magnet for attracting new patients and the world’s greatest oncological talent. With Mobetron, we’re accelerating the cure.
Learn More about the Mobetron
Let’s talk about how Mobetron will be the advantage in your facility’s comprehensive strategy for treating pancreatic cancer.

